In early July, over 200 scientists from 32 countries called for the medical community and national and international bodies to take airborne transmission of Covid-19 seriously. Research shows, they said, “beyond any reasonable doubt” that breathing, talking and coughing releases microdroplets that remain in the air, and Covid-19 particles carried in those microdroplets could infect people several metres distant. They called for measures to prevent such transmission, and said that with lockdown policies ending, an inadequate understanding of transmission routes among governments and public health bodies could have grave consequences.
The WHO then acknowledged for the first time the possibility of airborne transmission of the coronavirus, saying it was revaluating the evidence and planned to update its prevention guidelines.
Yao Maosheng of the Bioaerosol Laboratory at Peking University’s College of Environmental Sciences and Engineering, told the media that airborne transmission has been widely discussed in China, where it is referred to as aerosol transmission.
An aerosol is a persistent suspension of airborne particles less than 100 micrometres in size – smog and fog are both examples. Aerosols containing microorganisms or biological material such as viruses, bacteria, fungi, pollen and animal proteins are referred to as bioaerosols. SARS-CoV-2, the virus causing the Covid-19 disease, with a diameter of less than 0.1 micrometres, can be transmitted through the air when carried on an aerosol of dust or droplets. Aerosols are varied and present a wide range of risks – both epidemiological and environmental.
The airborne transmission debate
In Europe and the US a lot of public discussion has focused on whether wearing a mask in public is necessary to limit the possibility of airborne transmission of Covid-19. The WHO, US CDC and the UK government said there was no need to wear a mask unless you were unwell. But the possibility of asymptomatic carriers and transmission during the virus’s incubation period soon drew attention, while new research indicated that in poorly ventilated spaces the virus could remain suspended in the air for hours and travel significant distances. This all supported those advocating mask-wearing, and health authorities gradually moved to recommend the use of masks or other face coverings.
Antibiotic resistant genes spread very quickly in the air, and the development of new drugs can’t keep upYao Maosheng, Peking University Bioaerosol Laboratory
This was a debate that China had already had. In guidelines advising the public on how to prevent the spread of the virus published in late January, the Chinese Centre for Disease Control and Prevention listed three transmission routes: airborne transmission; close contact with an infected person; and transferring infected droplets via hands from surfaces to eyes, nose or mouth. Some said there was no conclusive evidence for airborne transmission while others said it was safer to assume there was. Regardless, airborne transmission was included in diagnosis and treatment guidelines issued later, but only as a possibility under certain circumstances.
An unusual cluster of SARS cases in a Hong Kong apartment block, the Amoy Gardens, during the 2003 outbreak were referred to as one reason for caution around airborne transmission. An investigation found the cluster may have been caused when the virus entered the sewer system of the building, became attached to droplets or particles forming aerosols, before finding its way into apartments via leaky pipes and dried-up U-bends. Although there is no conclusive evidence this was the route of transmission, it is a reasonable suspicion and should be taken seriously.
During an 8 February press conference on the coronavirus epidemic, one Shanghai official said the virus could spread by airborne transmission. Although no evidence for this was offered, it did lead to a general belief that this had been confirmed. Experts quickly pointed out a lack of conclusive evidence, but with the virus spreading quickly many people thought it was better to be cautious than await more evidence. A rapid increase in mask production made the debate less important and it was soon normal to wear a mask in public.

Chinese researchers have tried to find evidence of airborne transmission of the novel coronavirus. In early June, Yao Maosheng and his team published a preprint paper (a paper not yet peer reviewed and officially published) on medRxiv, which found normal respiration was an important source in the spread of the virus, alongside coughing and sneezing. A Covid-19 patient could exhale millions of virus particles every hour, in droplets smaller than 2.5 micrometres – smaller than those emitted by coughs and sneezes and so able to remain airborne for longer. This, the researchers said, explained why asymptomatic carriers of the virus, who did not cough or sneeze, could still infect others. They wrote: “Evidences from our work show that exhaled breath emission may well be the most significant SARS-CoV-2 shedding mechanism, which could have contributed largely to the observed cluster infections and the ongoing pandemic.”
Bioaerosols – an environmental issue
While the epidemic has raised concerns about aerosols, people in China were already familiar with the issue because of problems with smog, although the term bioaerosol was not much used.
In 2014, a group from Tsinghua University found 1,300 types of microorganism in Beijing’s smog although the majority were found to be harmless and very few could cause disease. In 2016, the international journal Microbiome published research finding antibiotic resistant genes in Beijing’s smog, causing public concern and leading experts to offer clarifications: finding the gene did not mean live antibiotic resistant bacteria had been found, and even live bacteria may not cause disease – and so there was no need for panic.
And perhaps there wasn’t, but according to a literature review published by Yao and others in 2018, livestock farms, wastewater treatment plants and hospitals can all release antibiotic resistant genes into the air, and those genes could be passed on to other bacteria when aerosols from different sources mix, creating a potential health risk. Yao told China Dialogue that they are currently looking at issues arising from these genes: “Antibiotic resistant genes spread very quickly in the air, and the development of new drugs can’t keep up with the speed at which bacteria acquire resistance via pollution.”
In 2018, Yao told Science and Technology Daily that bioaerosols are more easily absorbed into the body than chemicals and can, in certain conditions, breed, meaning there is no safe threshold for exposure. Research shows that fungi commonly found in the air such as penicillium, aspergillus and sporothrix can all produce allergens and cause allergic respiratory diseases. Exposure to bioaerosols also causes blood pressure to rise in healthy people, and irreversible loss of lung function. Other research has found bioaerosols are denser on smoggy days, increasing the health risks.
And sometimes bioaerosols can have more direct health consequences. Last November almost 100 employees at a veterinary institute in the northwest province of Gansu caught brucellosis. An investigation identified the source: a vaccination plant upwind of the institute was releasing an infected bioaerosol, which the staff had breathed in.
Research has found that when controlling for smoking, workers in the meat and livestock sectors have a higher risk from lung cancer – possibly from long-term exposure to high levels of bioaerosols. Other research shows the microorganisms in bioaerosols can affect the particulate matter in the atmosphere, changing the properties of allergens and promoting the development of allergies.
All this means bioaerosols are both a public health issue and an environmental issue, and that rapid bioaerosol monitoring and alerts are necessary.
Monitoring problems
The coronavirus pandemic means there is public and scientific interest in monitoring bioaerosols.
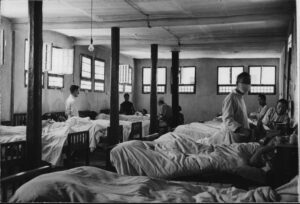
On 8 February, as China began a belated return to the cities after an extended Chinese New Year break, Chinese NGO Toxics Free Corps joined with other green NGOs including Natural Field and the China Biodiversity Conservation and Green Development Foundation to issue an urgent call for monitoring and publication of virus levels in the air at busy locations, in order to prevent airborne transmission. But China Dialogue has learned that while monitors were installed in some hospital wards and immigration halls, the only monitoring at transportation hubs was in Shenzhen, where the local disease control centre carried out monitoring at train and bus stations. According to Mao Da, founder of the Toxics Free Corps, the joint call did result in one member of the Qinhuangdao people’s political consultative committee suggesting monitoring, but no more.
The field requires inter-disciplinary knowledge, but electronic engineers don’t understand microorganisms and atmospheric scientists don’t know anything about virusesYao Maosheng, Peking University Bioaerosol Laboratory
Yao Maosheng also pointed out that hospitals, livestock farms, landfill sites and water treatment plants are all key sources of bioaerosols, but there is no monitoring there of disease-causing bacteria or allergens.
Yao explained that this is due to difficulties with such monitoring. Microorganisms are not like chemicals – they are more varied, even including as-yet unidentified species. Countries that do carry out monitoring, such as France, only check for allergens.
Currently, China does not have any suitable methods for monitoring bioaerosols. During the monitoring in Shenzhen a traditional approach using a buffer solution to absorb viruses from the air for later laboratory analysis was used. This was called into question online as being too slow. Equipment developed by Yao and his team can detect flu viruses such as H3N2, H1N1 and H5N1, but specific modules need to be developed for other viruses.
Bacteria, another important constituent of bioaerosols, are most often detected with ultraviolet lights. Yao told China Dialogue that this method is cheap but has problems: it can cause false positives where chemical particles are identified as bacteria, does not identify a specific type of bacteria, and can suffer interference from the background environment. His lab is working on a new method that will be more accurate, but require expensive reagents and professional maintenance. He sees an urgent need for a fast and sensitive monitoring method that can identify a wide range of bacteria.
Basic research overlooked
There are many challenges facing research into bioaerosols. Yao told China Dialogue that the field requires inter-disciplinary knowledge. “But usually, electronic engineers don’t understand microorganisms, people working on detecting microorganisms don’t understand environmental issues, and atmospheric scientists don’t know anything about viruses,” he said.
Another issue is the pursuit of higher “impact factor” within academic publishing, and a lack of state interest in some fields.
Deng Weiwei, a professor at Southern University of Science and Technology’s Department of Mechanics and Aerospace Engineering, wrote in February that basic research into bioaerosols has been neglected. Because, Deng said, the “fairest” but least useful method of displaying academic influence is looking at the impact factor of a paper, which uses citations as a proxy for importance. Research into bioaerosols would be published in a specialist journal and not the applied science journals that have higher impact factors.
Yao said he isn’t too worried about impact factors, and that papers published in top international journals aren’t necessarily more valuable than those in specialist journals on bioaerosols. “If research makes a contribution to society, people will see it, even if you just post it on WeChat.”